billing
Manage billing
while reducing
errors and delays
ABA Matrix streamlines every step of billing—from claim generation to payer compliance, clearinghouse integration, and financial reporting. With automated workflows, payer-specific configurations, and real-time claim tracking, your practice can reduce errors, accelerate payments, and maintain full visibility over your revenue cycle.
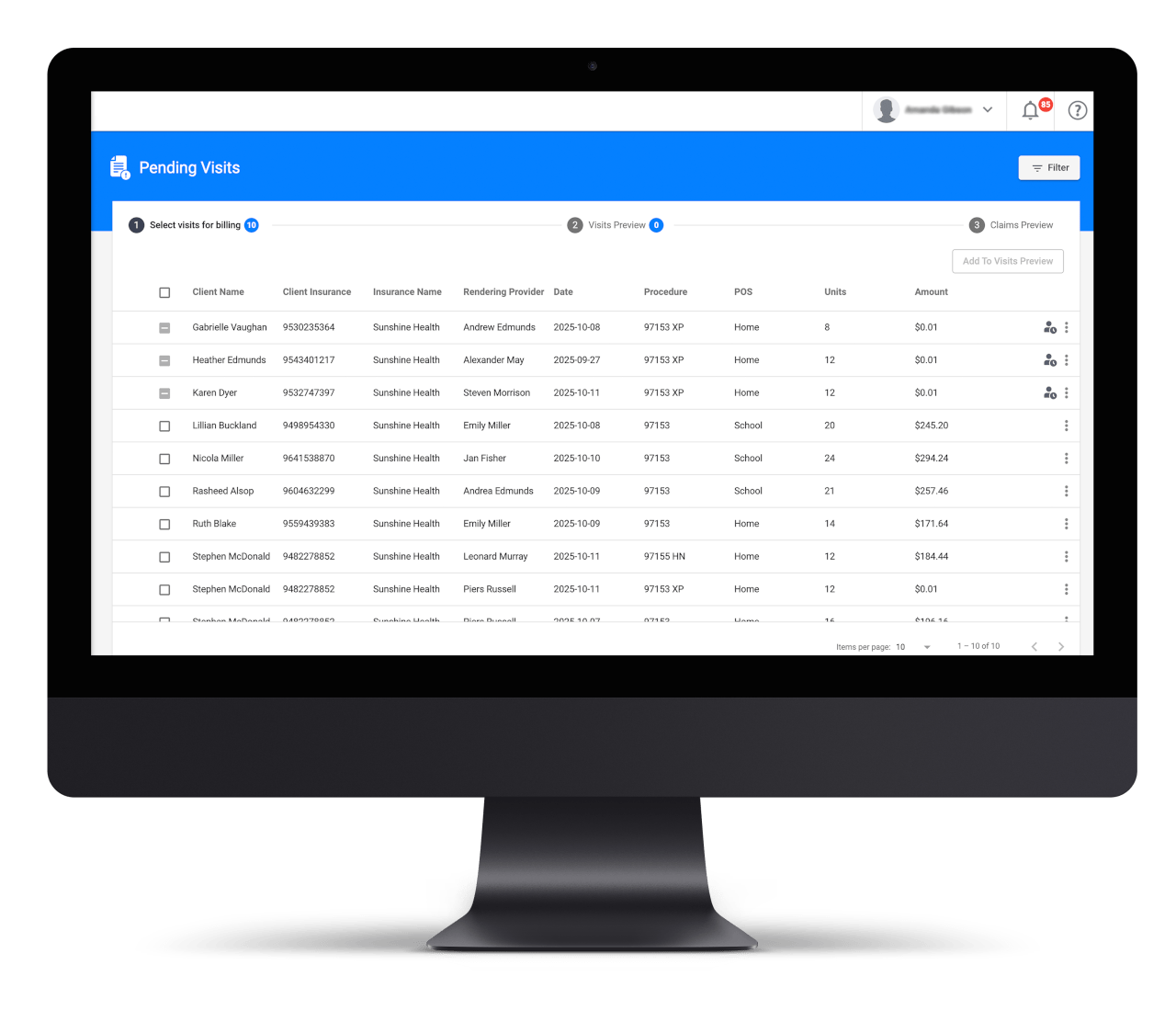
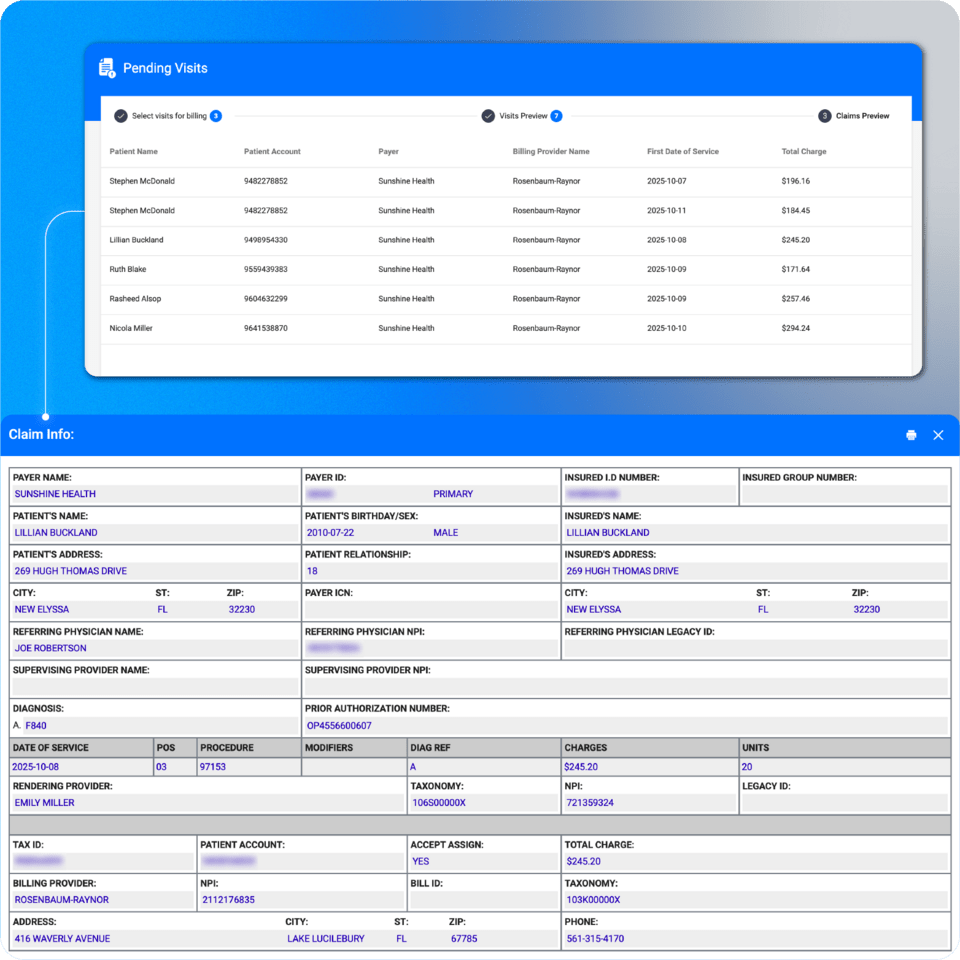
Claim generation
Claim generation
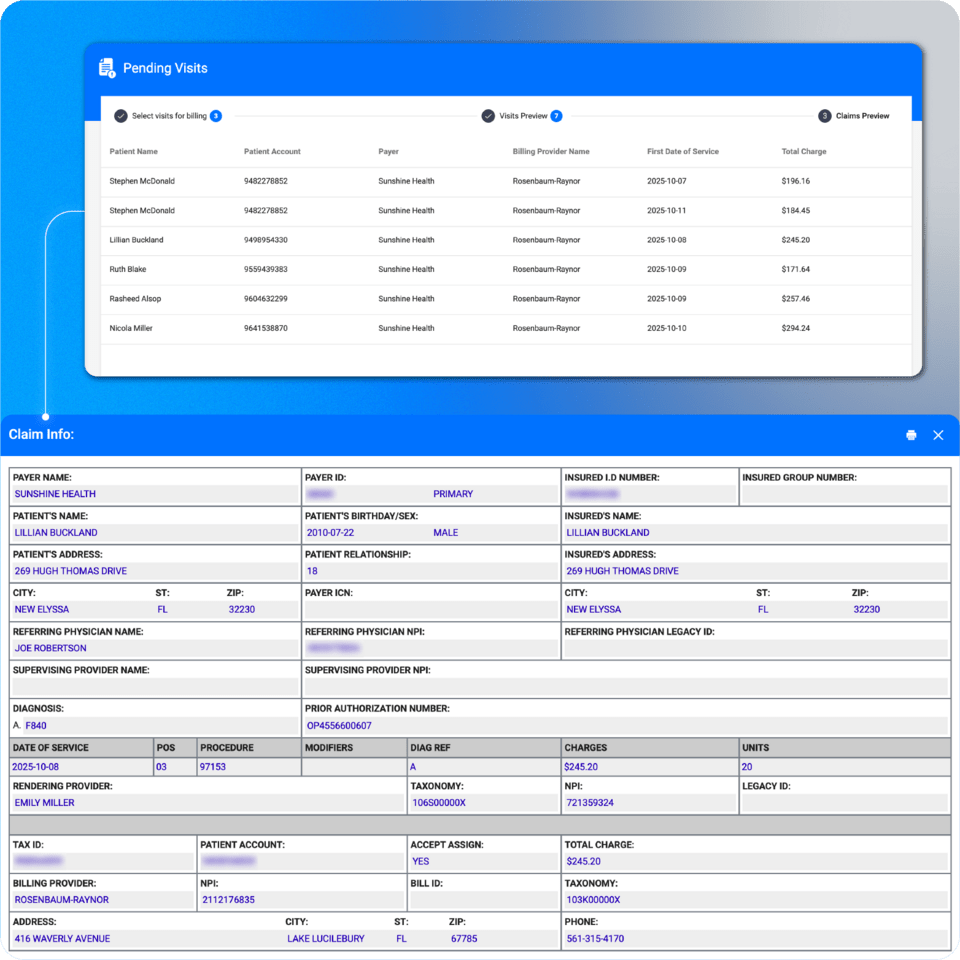
In ABA Matrix, once a visit is completed, it automatically moves to the Pending Visits section in Billing. From there, users can select the visits, and a claim will be generated using existing information such as insurance details, units, procedure codes, rendering provider, billing provider, and more. With our billing feature, users will never need to enter the same information twice, making the process more efficient, accurate, and less prone to errors.
Insurance/payer management
Insurance/payer management
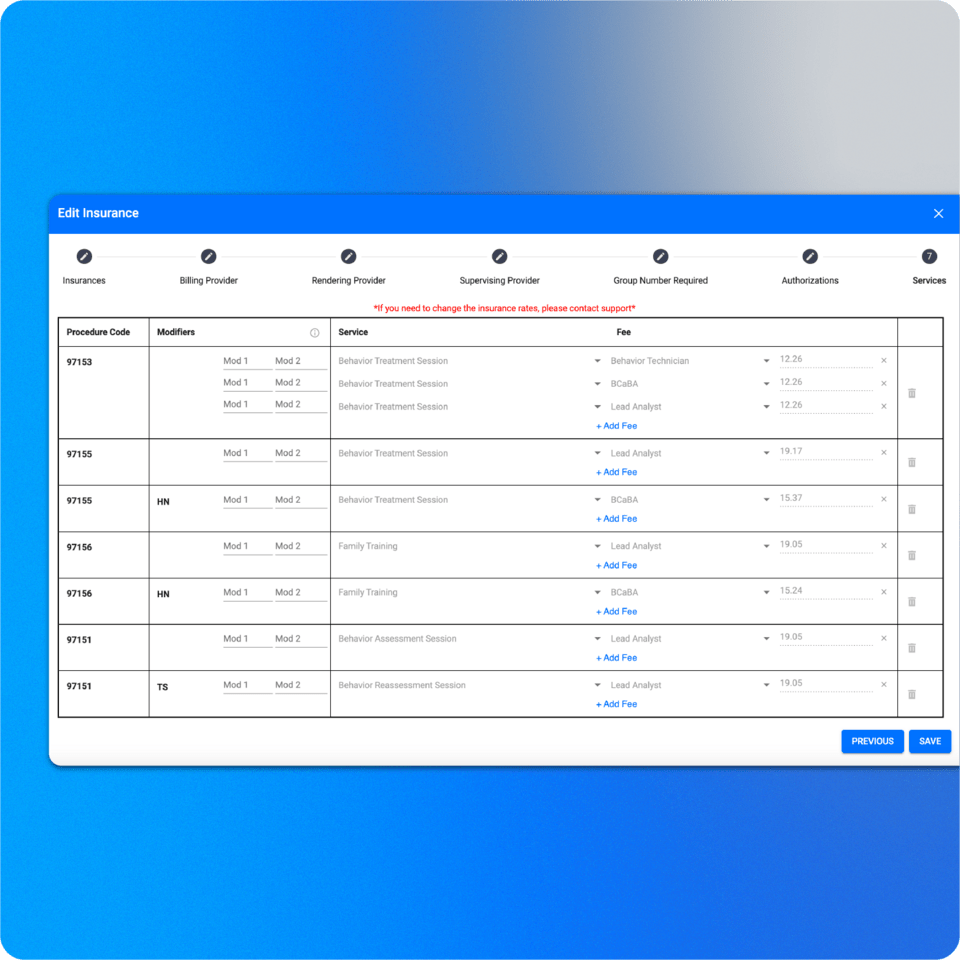
Users can configure all the payers their organization is in-network with, including their fee schedules, allowable services, and required provider certifications for each procedure. Once set up, they can assign a payer to a client—along with their copayment and coinsurance details—, and ABA Matrix will automatically apply the correct rate, payer, and procedure code whenever a provider schedules a service. This minimizes errors and streamlines the scheduling process.
Payer-specific claim configurations
Payer-specific claim configurations
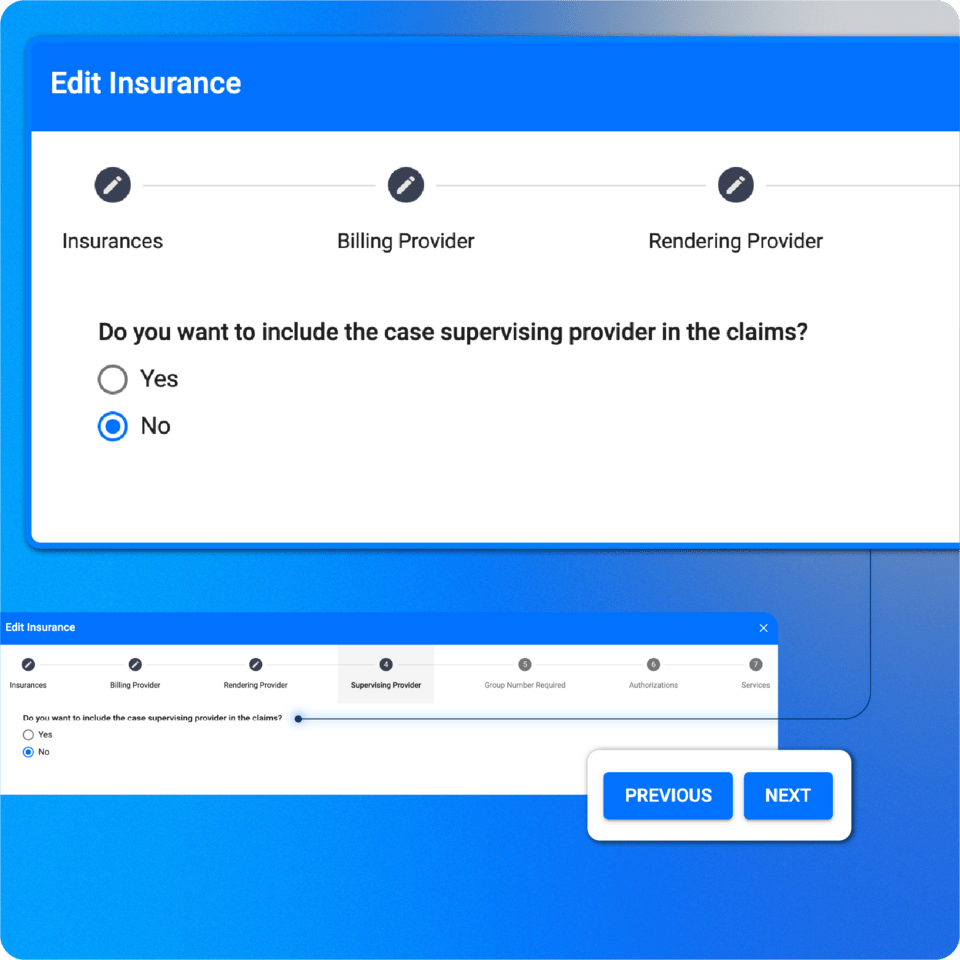
In ABA Matrix, users can preconfigure how claims are constructed based on each payer’s specific requirements. When setting up a payer, they can choose whether to include details such as the payer address, case supervising provider, insurance group number, and other claim elements. This ensures claims are always aligned with each payer’s compliance standards.
Clearinghouse integration: fully integrated with Claim.MD (Optional)
Clearinghouse integration: fully integrated with Claim.MD (Optional)
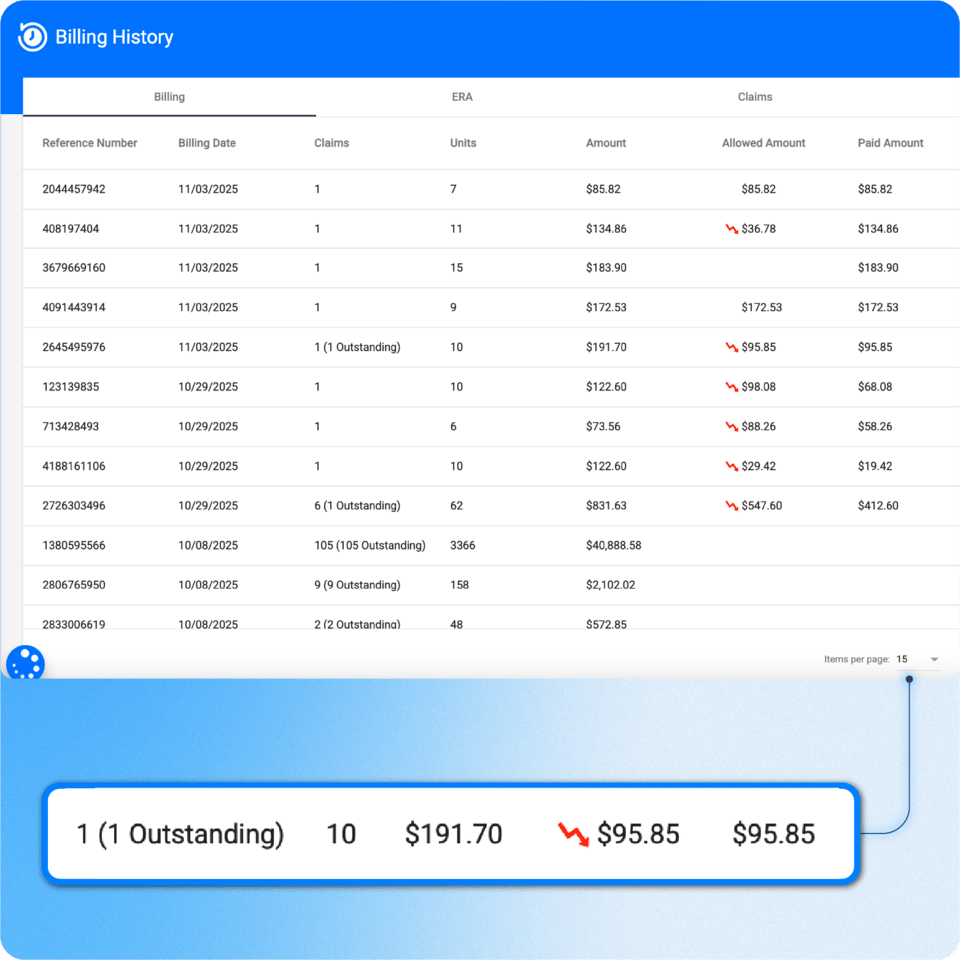
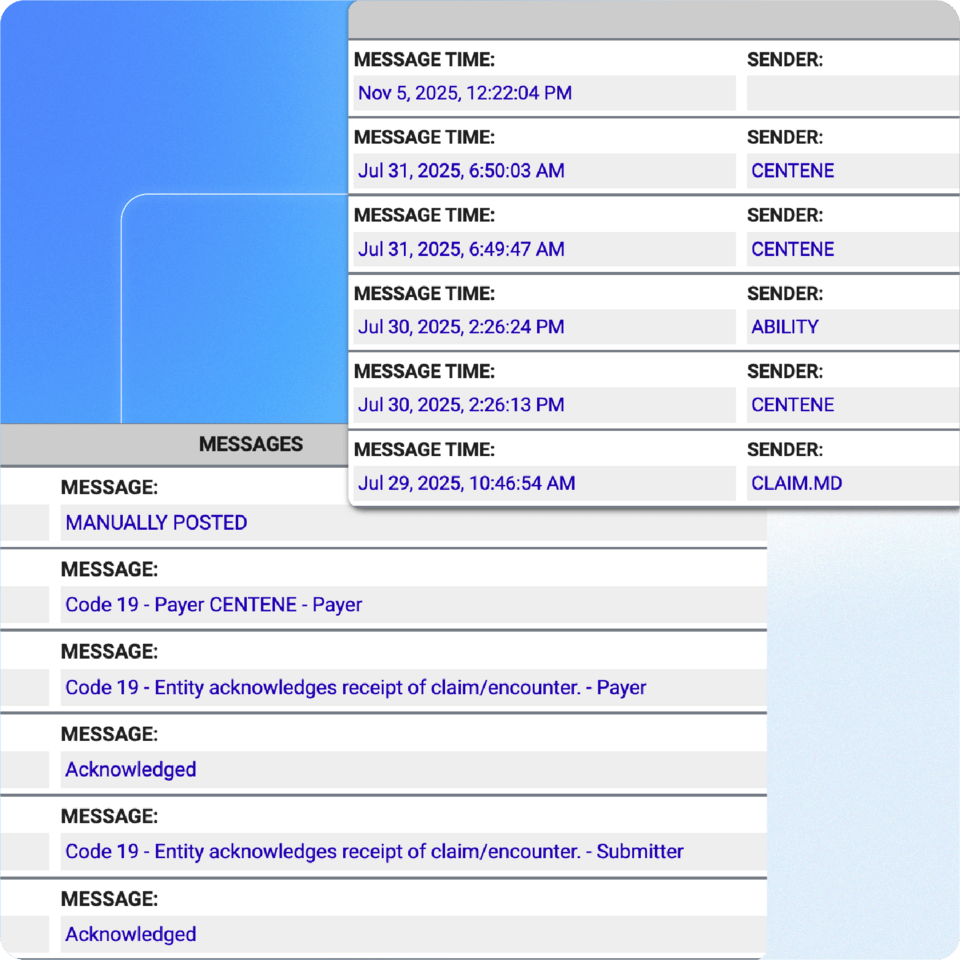
With our ClaimMD integration, users can submit electronic claims to thousands of payers, receive Electronic Remittance Advices (ERAs), and run real-time eligibility checks directly from ABA Matrix:
- Automatic posting: Through the ClaimMD integration, ABA Matrix uses ERAs and claim messages to automatically post payments and denials. This ensures users never miss a payment and keeps the billing process efficient and accurate.
- Denials management: From our Denied and Rejected screen, users can view all claims that have been denied or rejected, along with the specific reasons. Users can also correct and retransmit the affected claims directly from this screen, streamlining the resubmission process.
- Real time claim status: Users can request real-time claim status updates from participating payers. If a claim has been outstanding, they can check its current status directly within ABA Matrix in just seconds, saving time and improving follow-up efficiency.
Non-integrated claim management
Non-integrated claim management
Even if a user chooses not to utilize the optional Clearinghouse Integration, they can still take full advantage of our billing features. Users will be able to create claims and batches, obtain reports, and manually post payments or denials as needed.
Comprehensive financial reports
Comprehensive financial reports
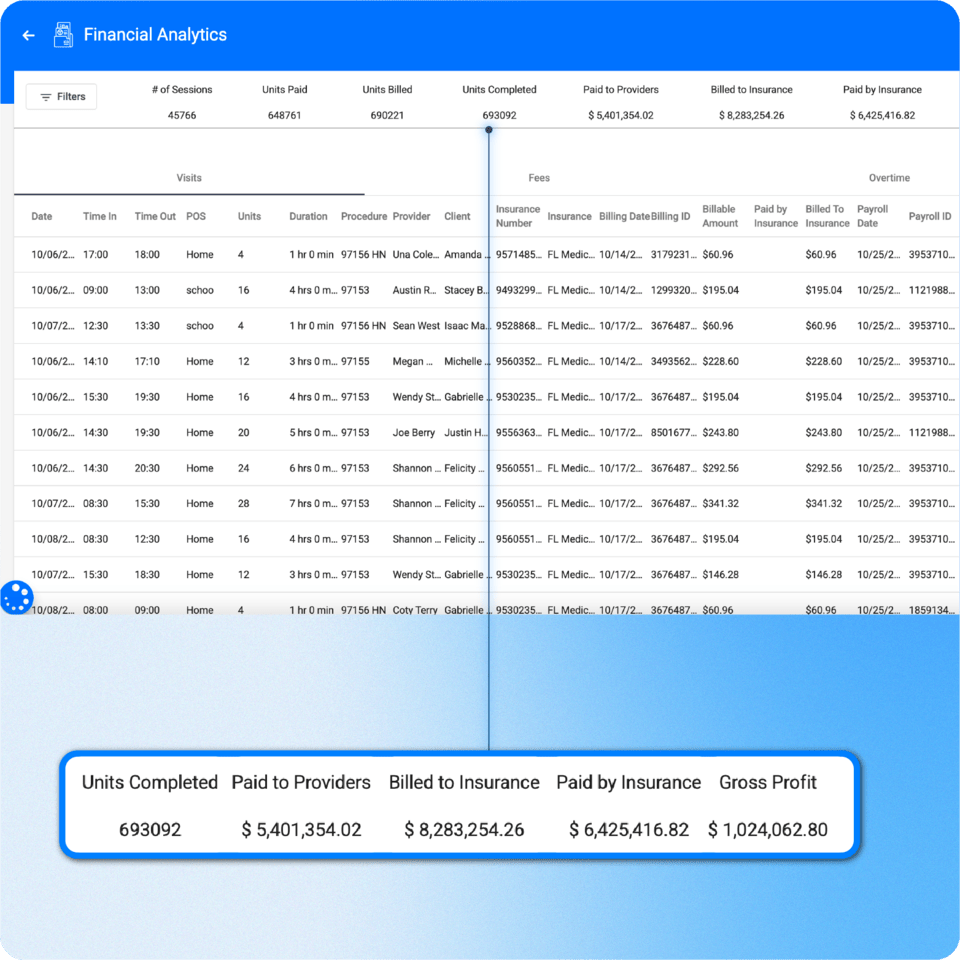
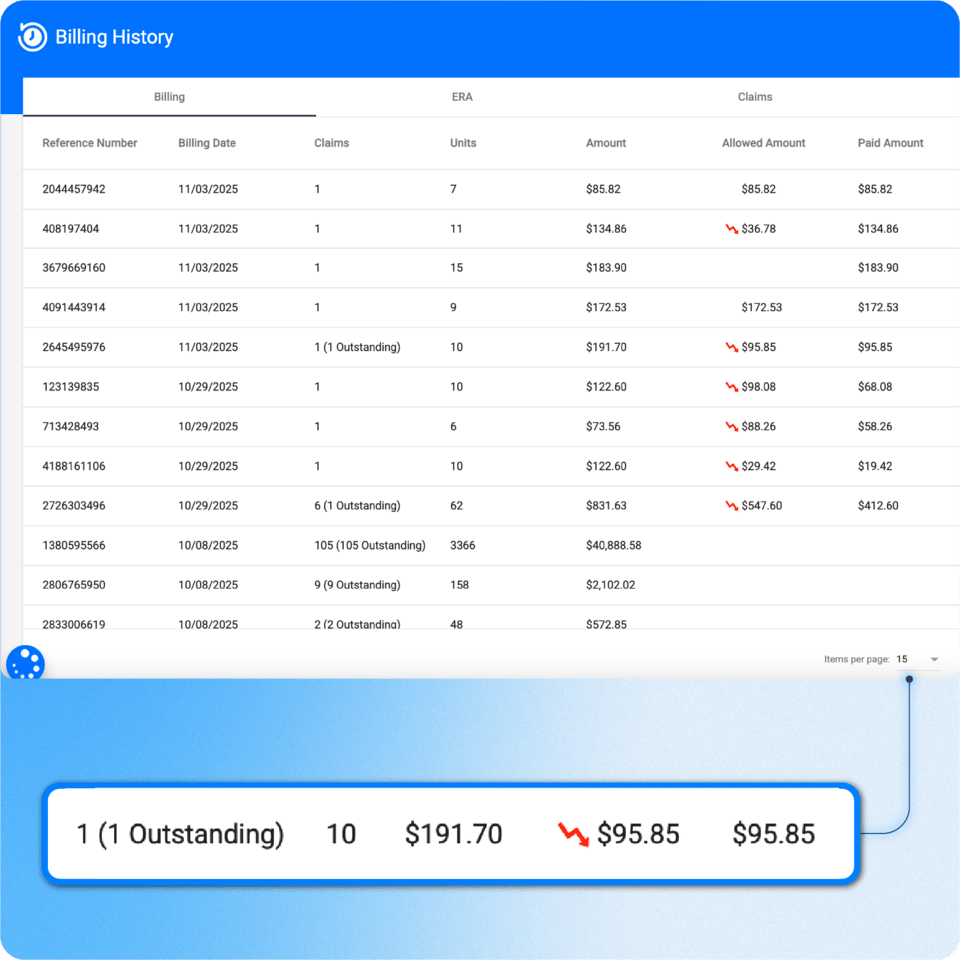
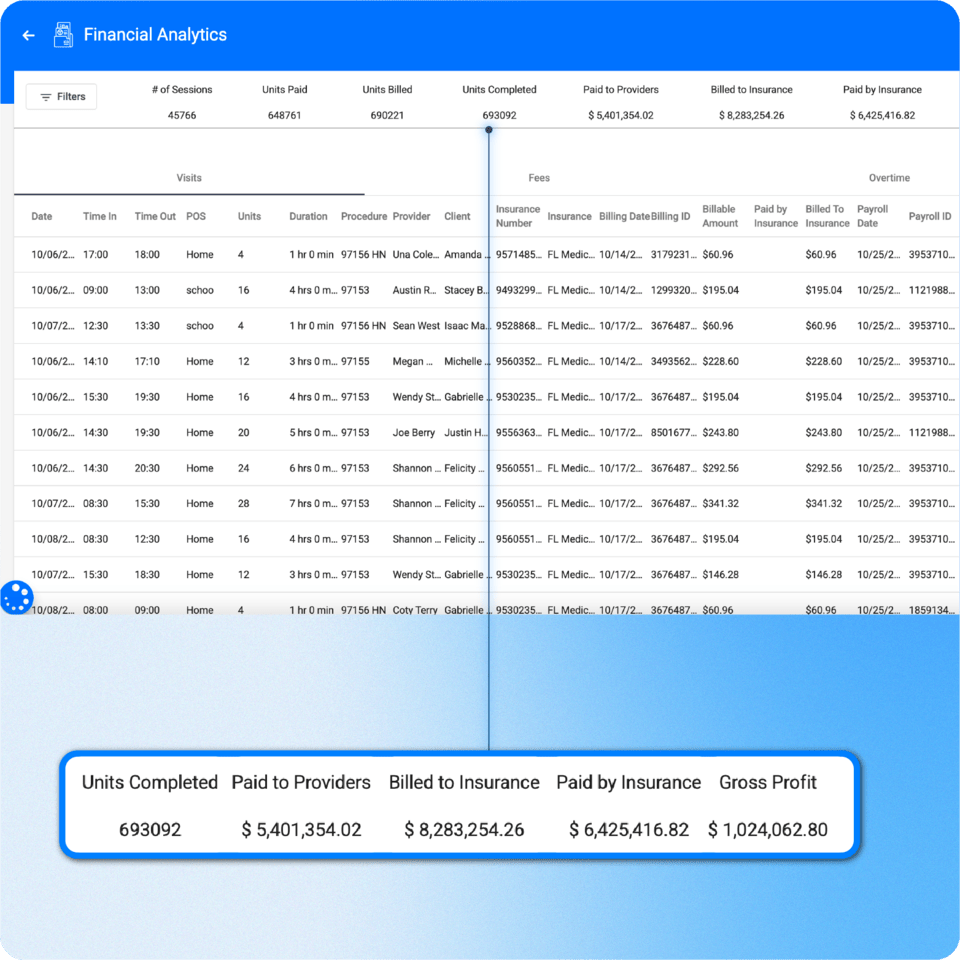
In ABA Matrix, users have access to comprehensive and advanced financial analytics, including profit tracking and detailed session breakdowns segmented by time period, provider, client, claim status, and service code for enhanced clarity and actionable insights.
Claim generation
Claim generation
In ABA Matrix, once a visit is completed, it automatically moves to the Pending Visits section in Billing. From there, users can select the visits, and a claim will be generated using existing information such as insurance details, units, procedure codes, rendering provider, billing provider, and more. With our billing feature, users will never need to enter the same information twice, making the process more efficient, accurate, and less prone to errors.
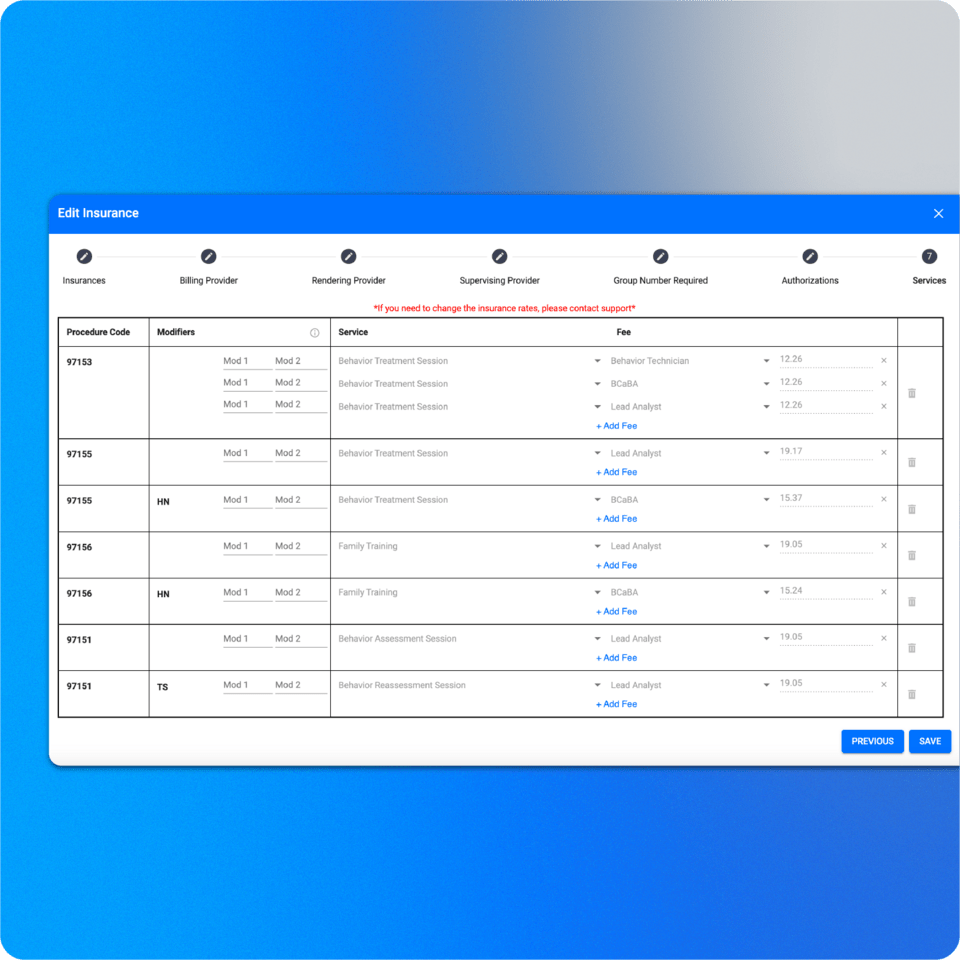
Insurance/payer management
Insurance/payer management
Users can configure all the payers their organization is in-network with, including their fee schedules, allowable services, and required provider certifications for each procedure. Once set up, they can assign a payer to a client—along with their copayment and coinsurance details—, and ABA Matrix will automatically apply the correct rate, payer, and procedure code whenever a provider schedules a service. This minimizes errors and streamlines the scheduling process.
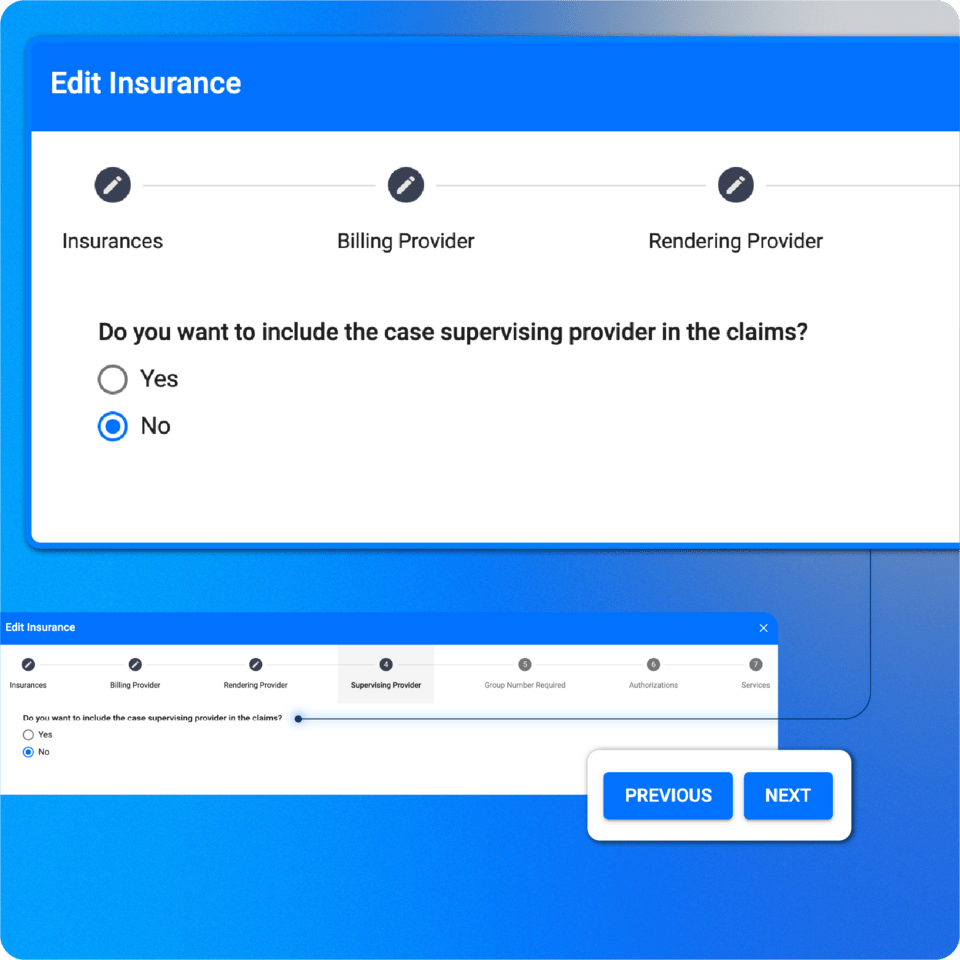
Payer-specific claim configurations
Payer-specific claim configurations
In ABA Matrix, users can preconfigure how claims are constructed based on each payer’s specific requirements. When setting up a payer, they can choose whether to include details such as the payer address, case supervising provider, insurance group number, and other claim elements. This ensures claims are always aligned with each payer’s compliance standards.
Clearinghouse integration: fully integrated with Claim.MD (Optional)
Clearinghouse integration: fully integrated with Claim.MD (Optional)
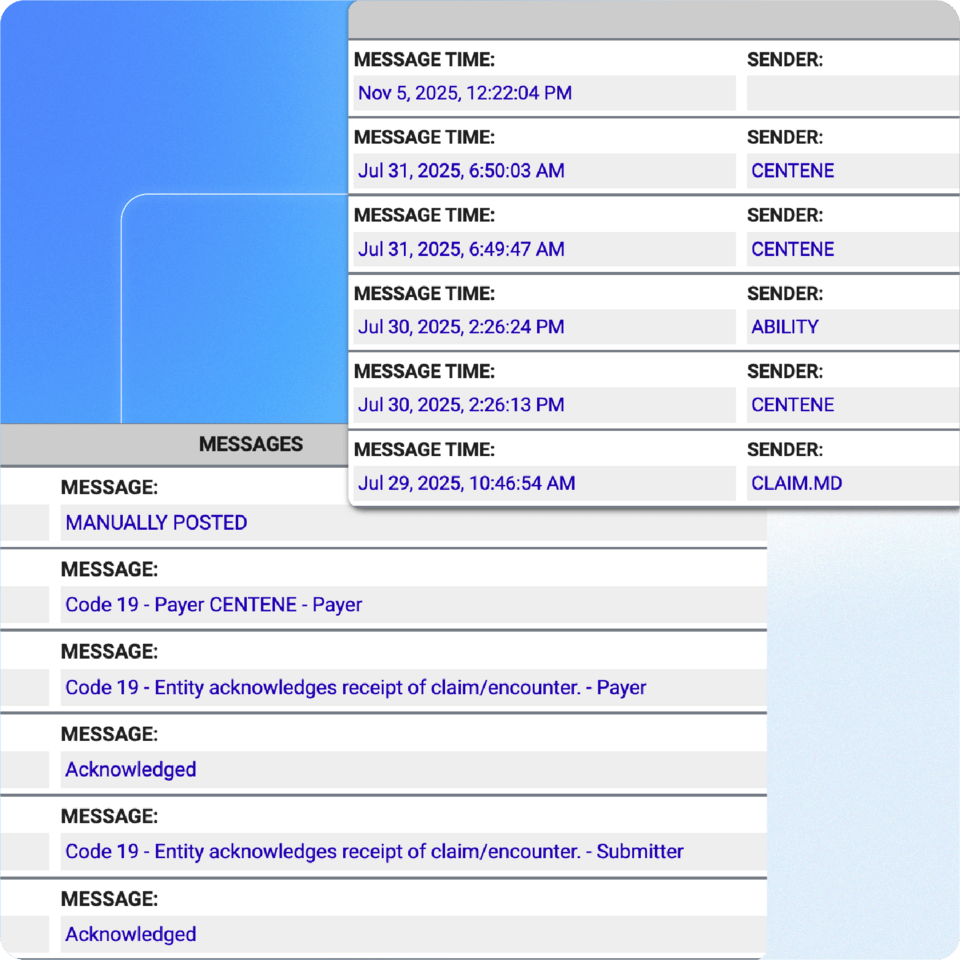
With our ClaimMD integration, users can submit electronic claims to thousands of payers, receive Electronic Remittance Advices (ERAs), and run real-time eligibility checks directly from ABA Matrix:
- Automatic posting: Through the ClaimMD integration, ABA Matrix uses ERAs and claim messages to automatically post payments and denials. This ensures users never miss a payment and keeps the billing process efficient and accurate.
- Denials management: From our Denied and Rejected screen, users can view all claims that have been denied or rejected, along with the specific reasons. Users can also correct and retransmit the affected claims directly from this screen, streamlining the resubmission process.
- Real time claim status: Users can request real-time claim status updates from participating payers. If a claim has been outstanding, they can check its current status directly within ABA Matrix in just seconds, saving time and improving follow-up efficiency.
Non-integrated claim management
Non-integrated claim management
Even if a user chooses not to utilize the optional Clearinghouse Integration, they can still take full advantage of our billing features. Users will be able to create claims and batches, obtain reports, and manually post payments or denials as needed.
Comprehensive financial reports
Comprehensive financial reports
In ABA Matrix, users have access to comprehensive and advanced financial analytics, including profit tracking and detailed session breakdowns segmented by time period, provider, client, claim status, and service code for enhanced clarity and actionable insights.
Simplify your billing and claims process
Connect with us and see how ABA Matrix can simplify your workflow