authorization management
Stay in control
of authorizations
Authorization management helps practices track, monitor, and validate authorizations with ease. From setup and real-time utilization tracking to automatic alerts and payer validation, the system ensures that your sessions stay compliant with coverage limits—reducing errors, preventing denials, and saving valuable administrative time.
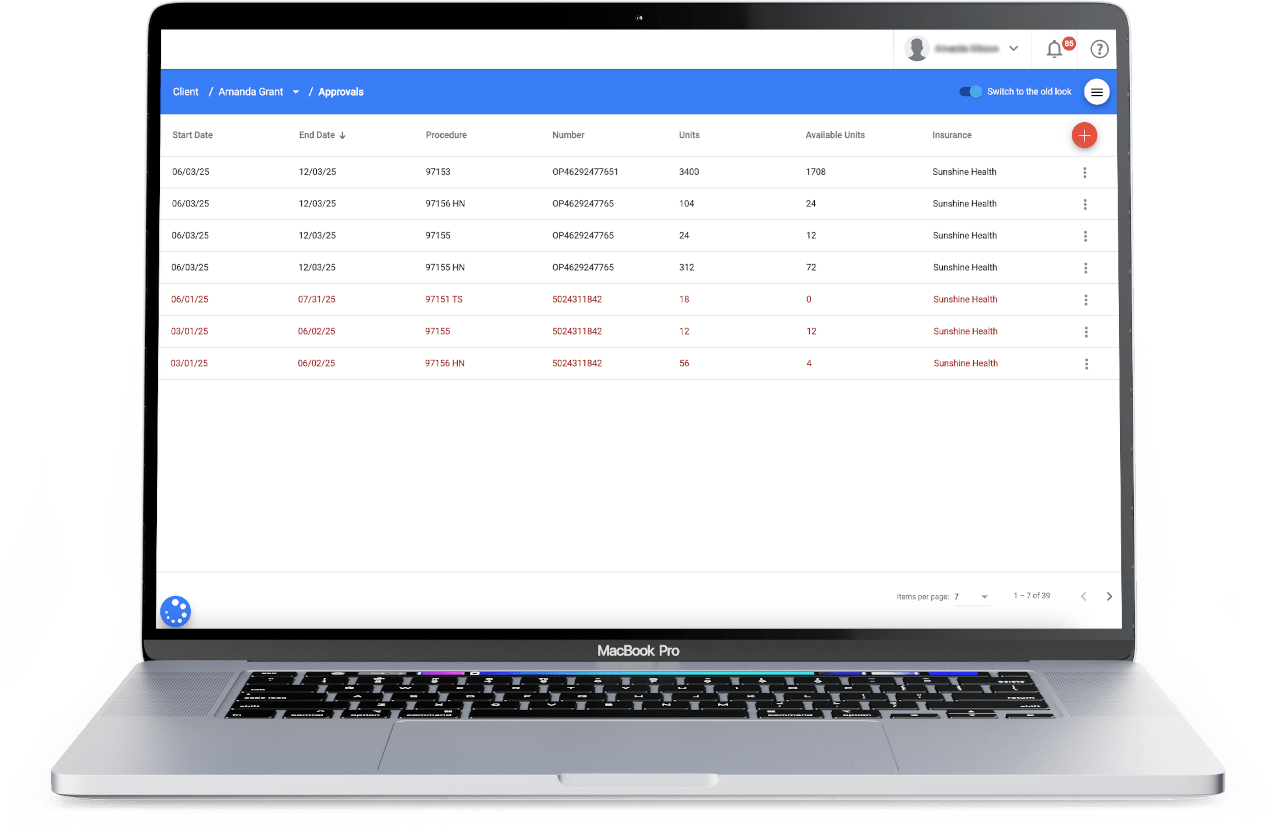
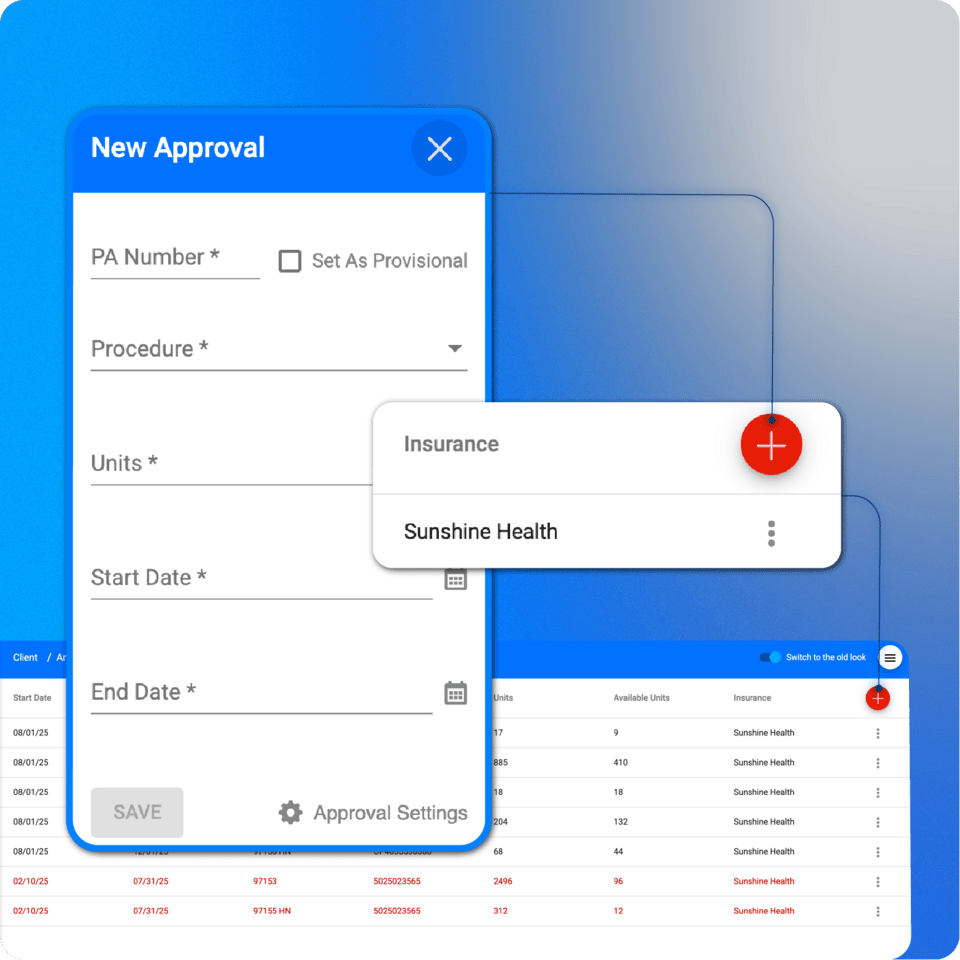
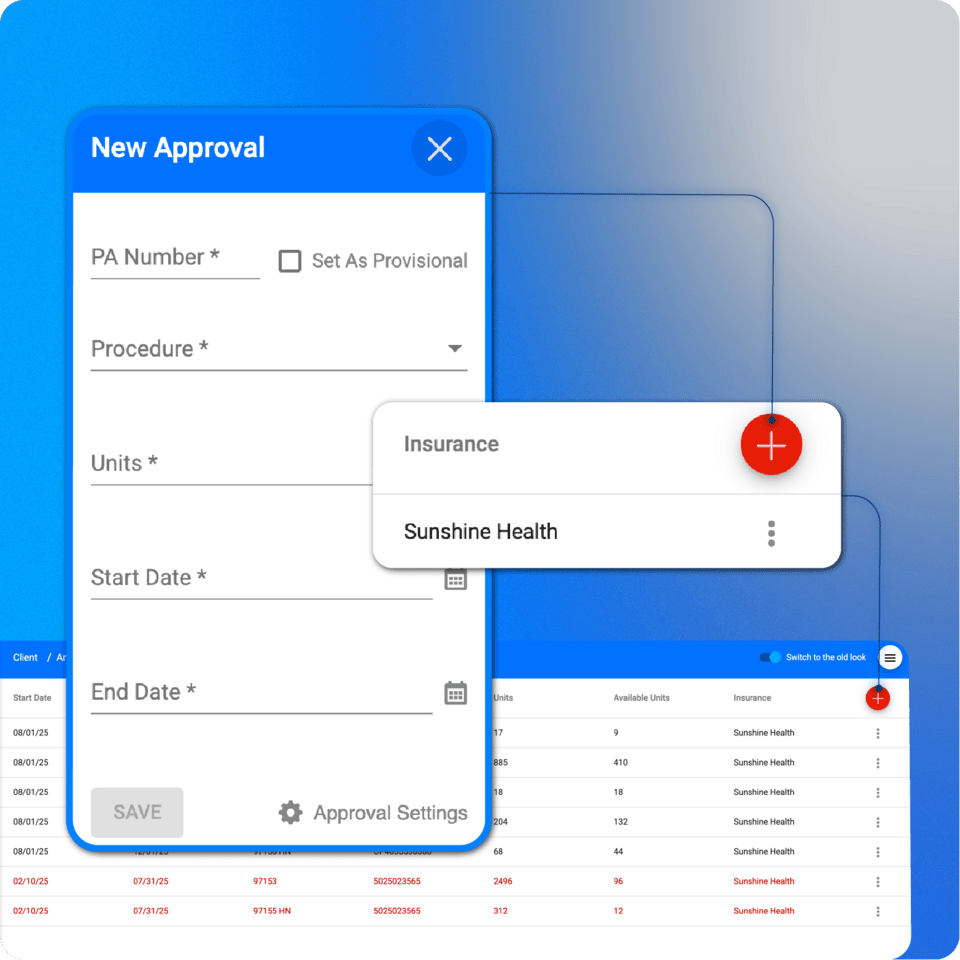
Authorization setup
Authorization setup
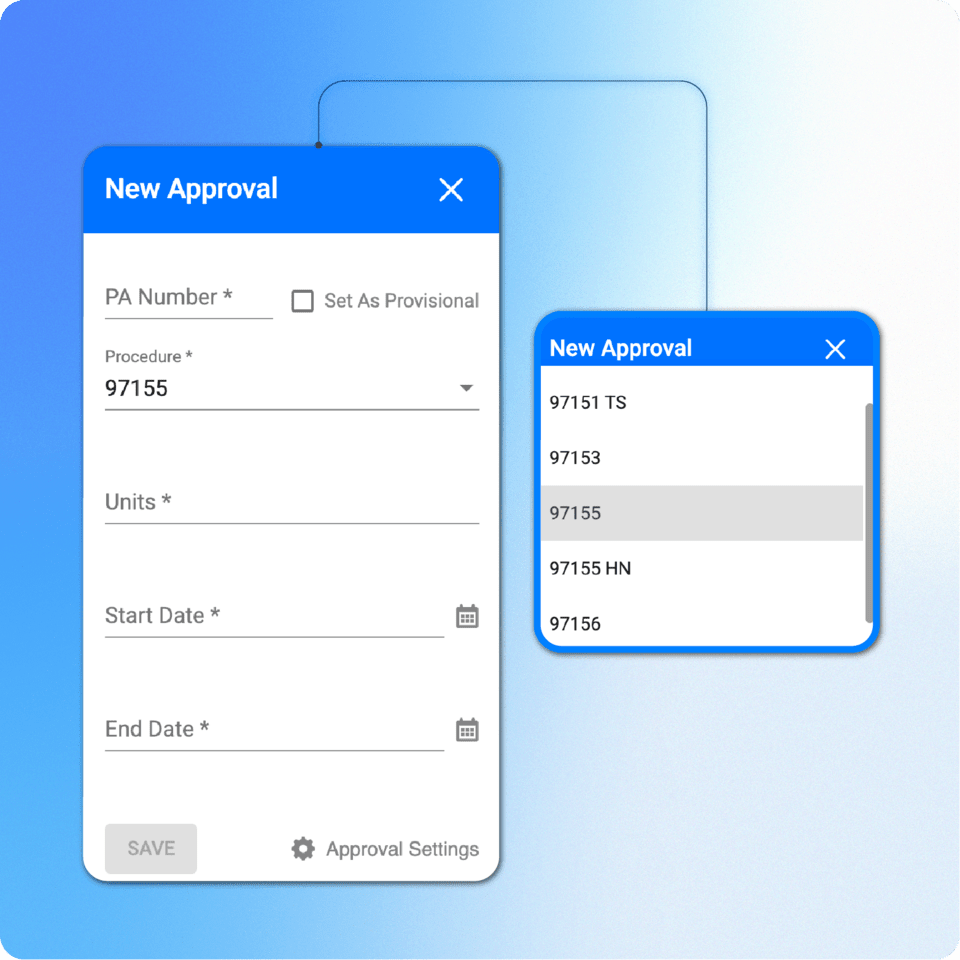
In ABA Matrix, users can add prior authorizations (PA) to the client’s profile, including units and approval periods.
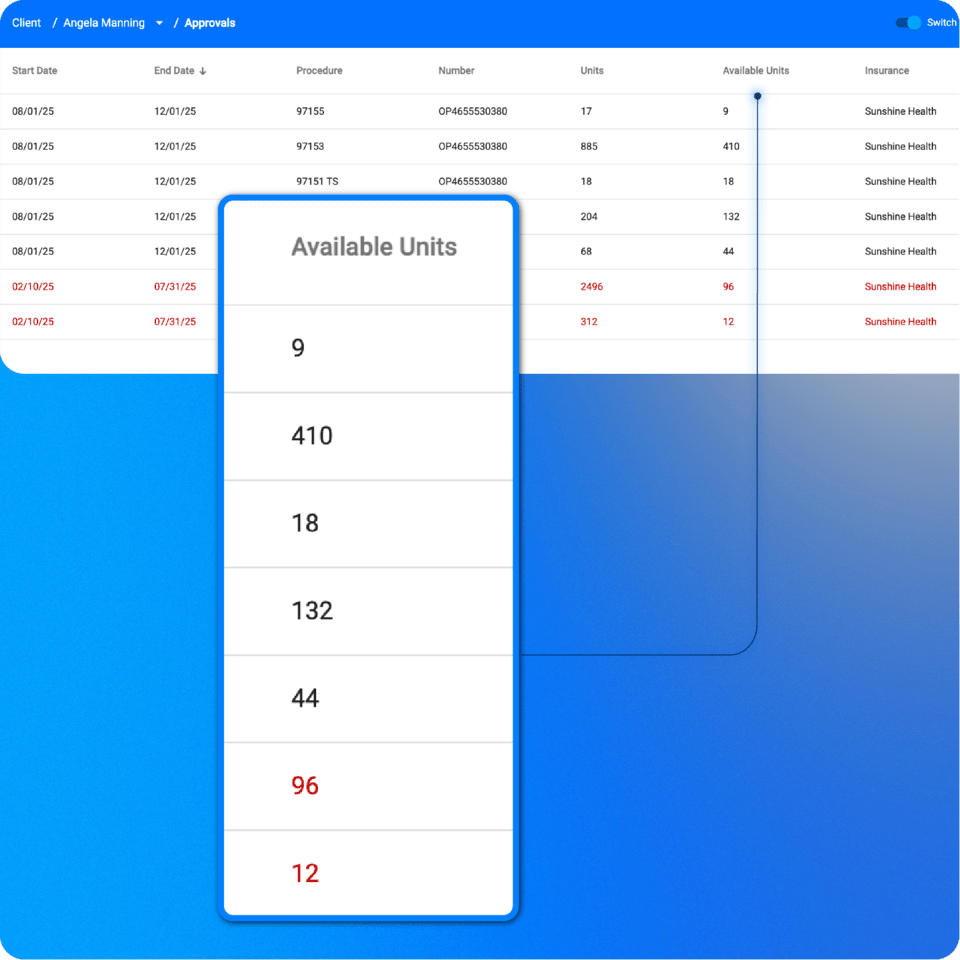
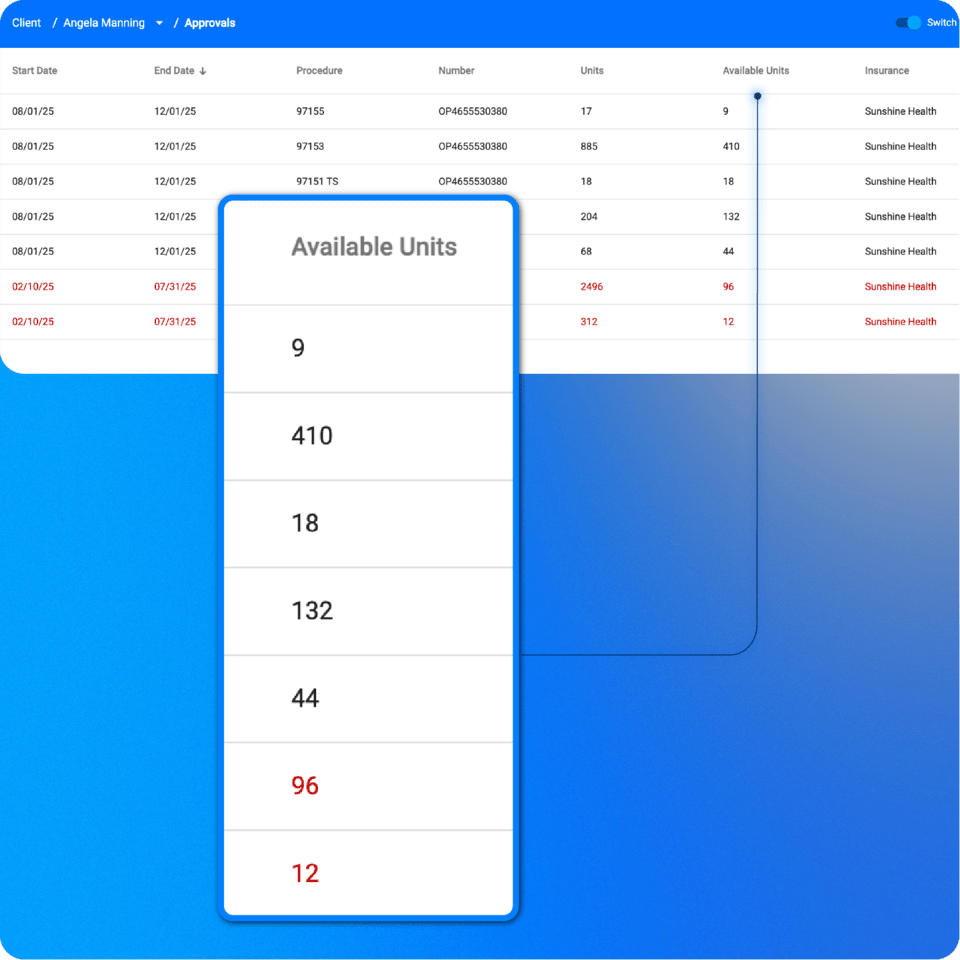
Authorization monitoring
Authorization monitoring
Users can monitor remaining authorized units in real time, with seamless integration to the calendar. As sessions are scheduled or updated, the system automatically adjusts the available units, ensuring an always-accurate view of each client’s authorization status.
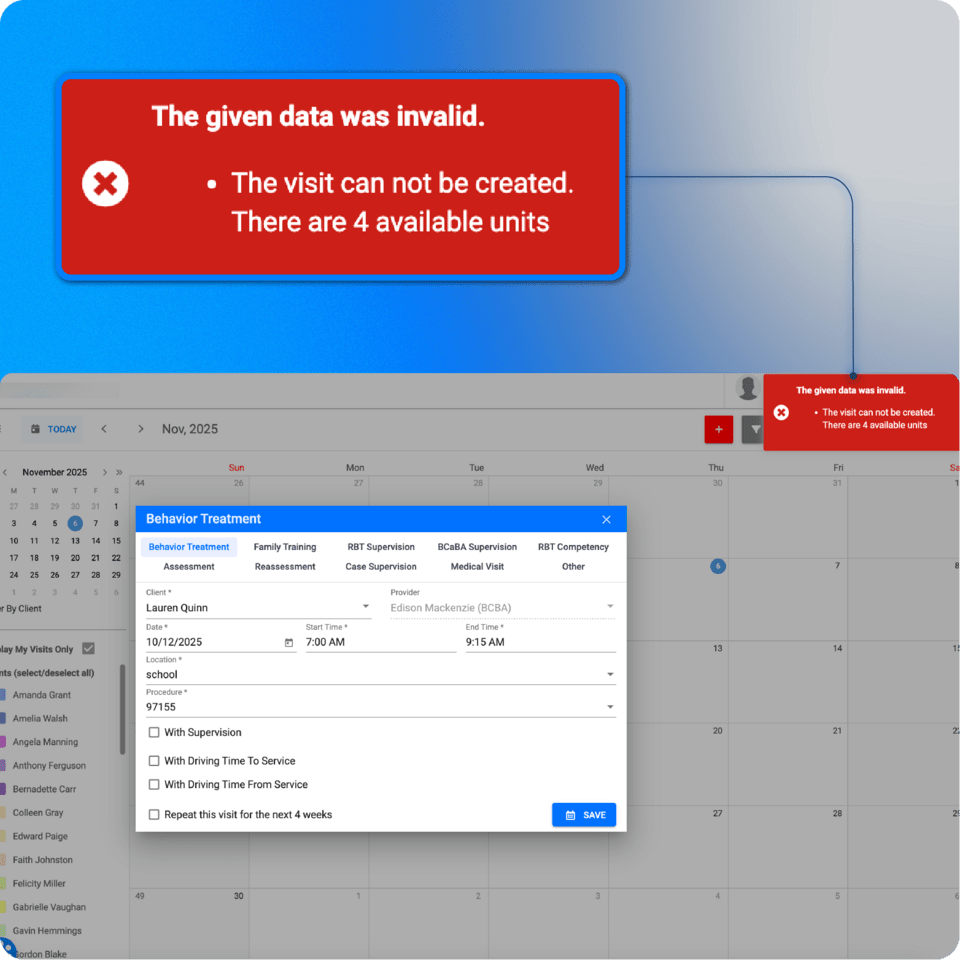
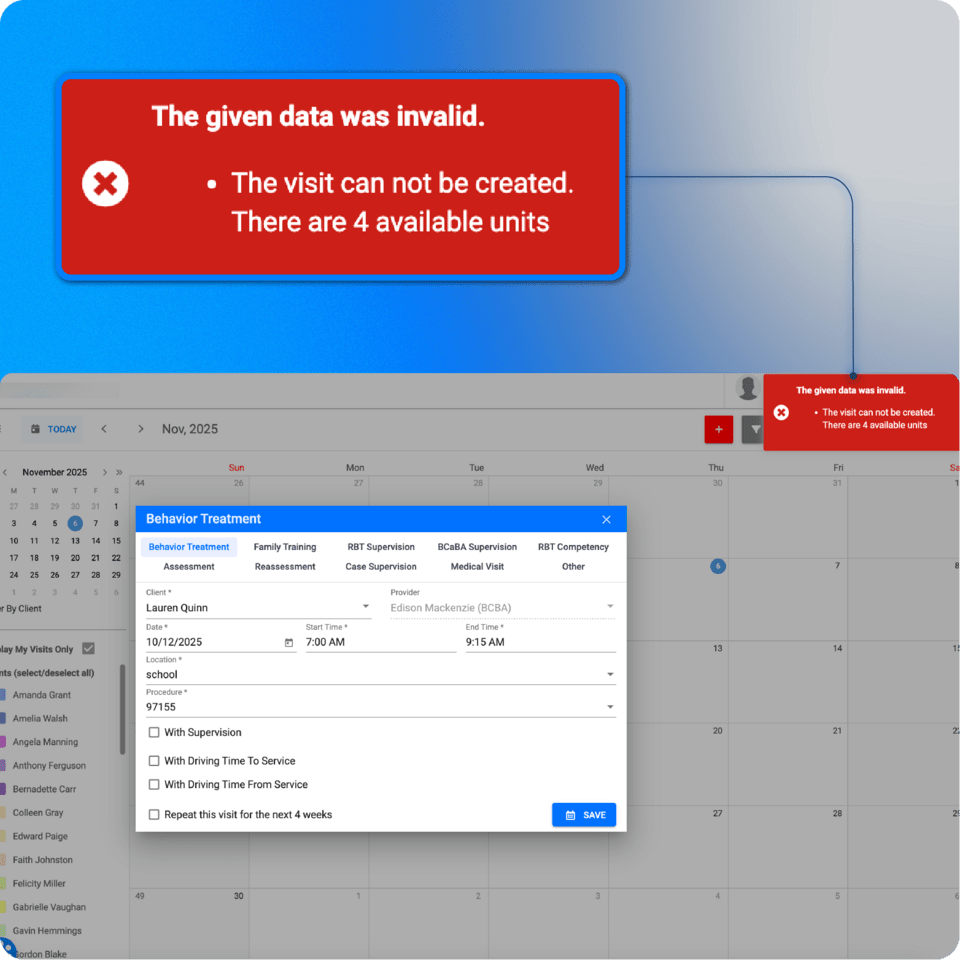
Overutilization prevention
Overutilization prevention
Users can prevent scheduling or billing when authorized units or periods are exceeded, ensuring that services are always within the coverage limits set by insurance.
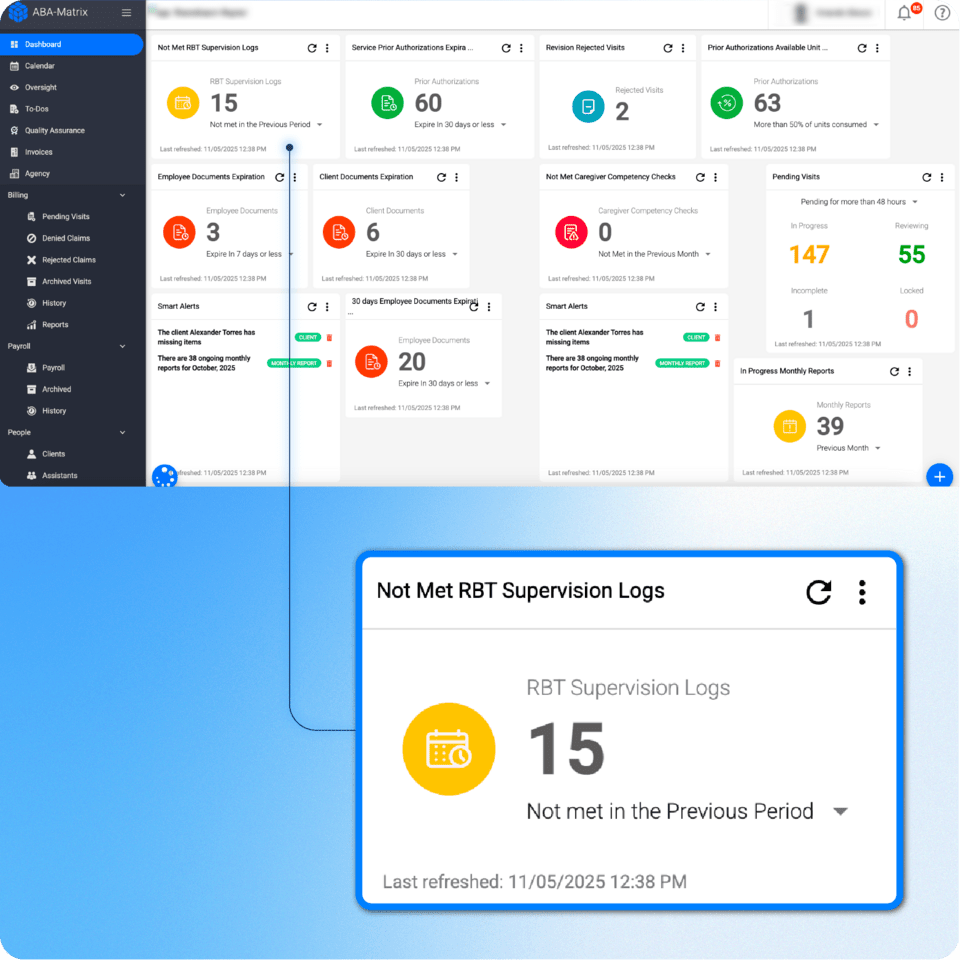
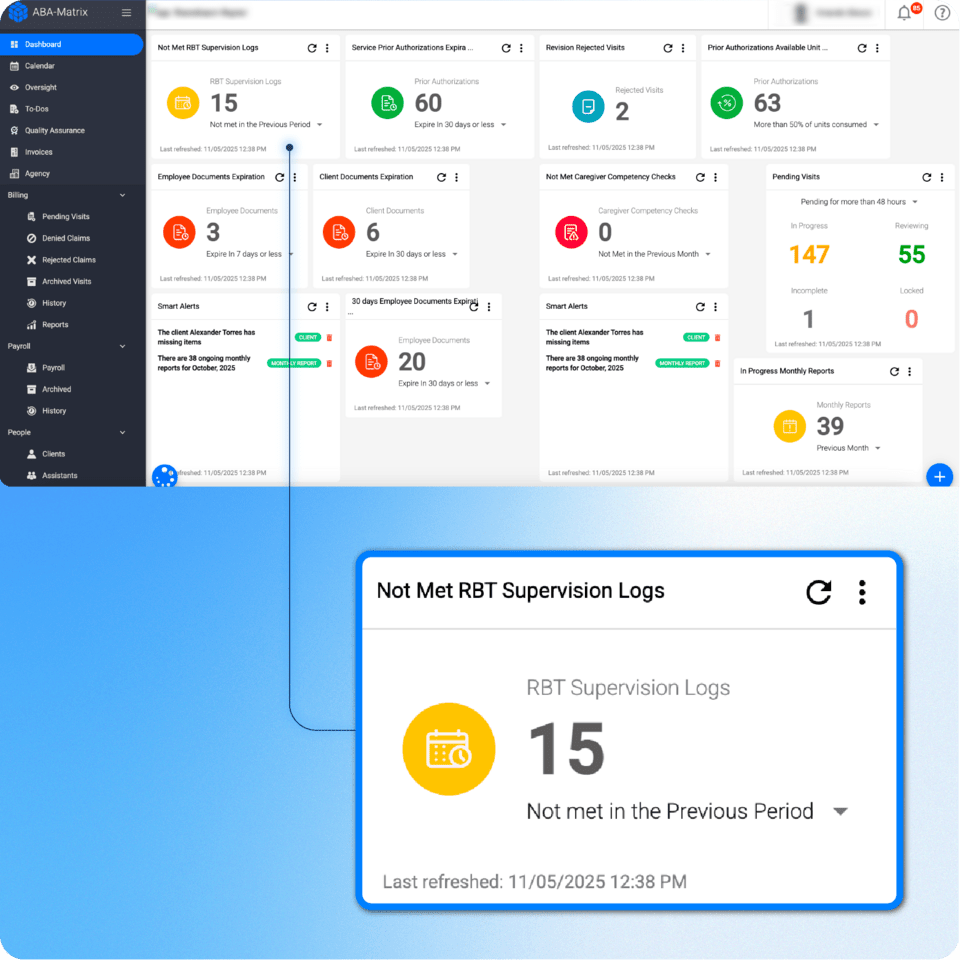
Utilization reports and dashboard alerts
Utilization reports and dashboard alerts
Users can access clear reports showing lost hours per week and remaining authorized units, and take a quick glance at the dashboard authorization alerts to keep ahead of any authorization running out of units or expiring.
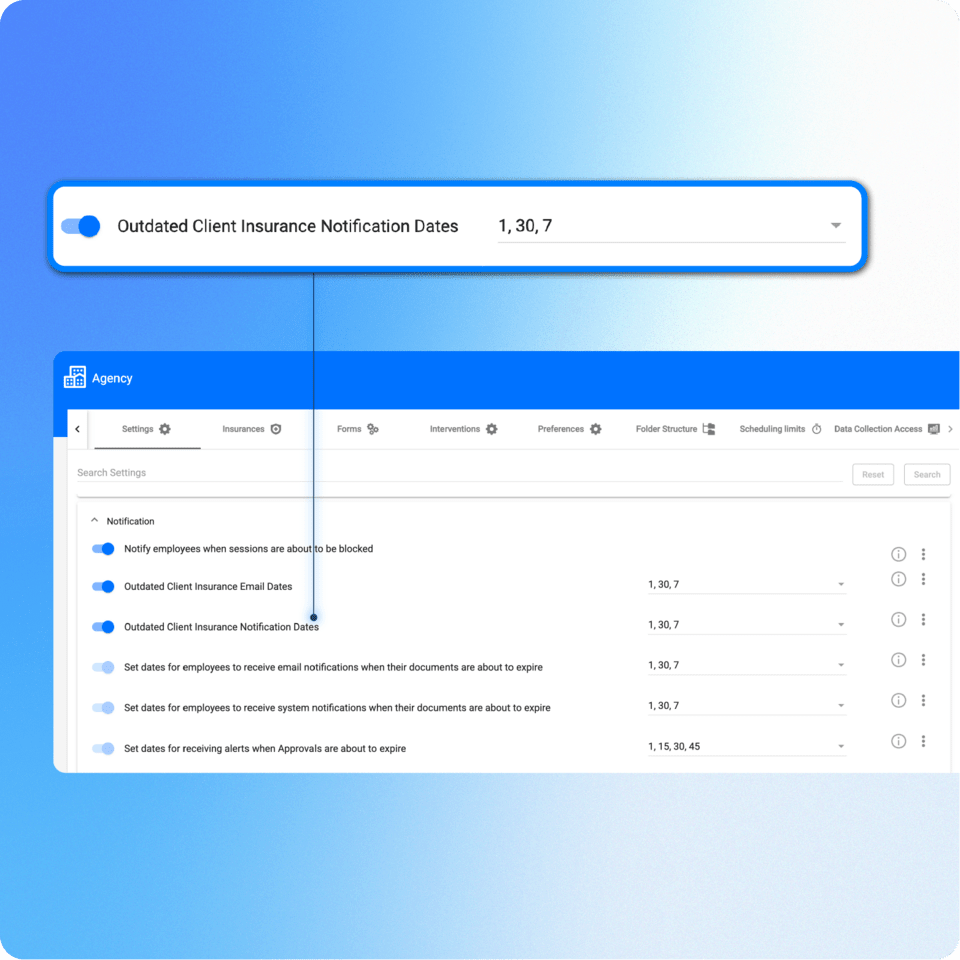
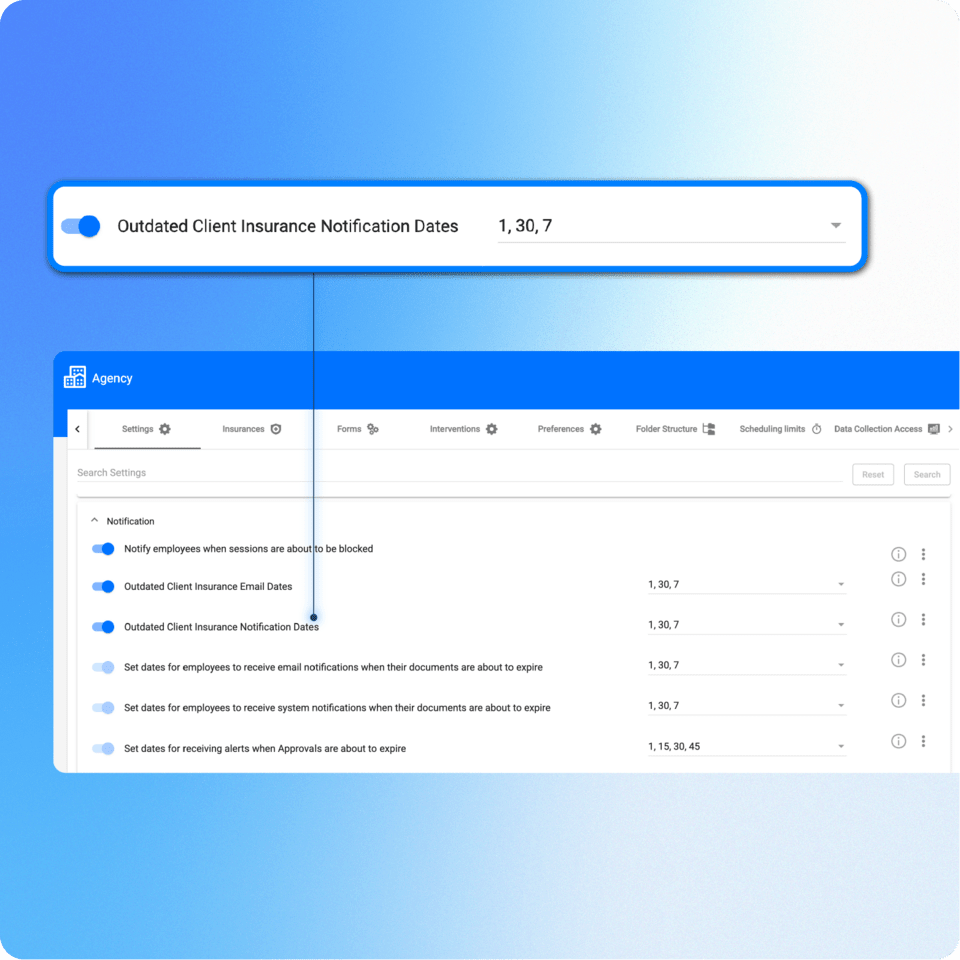
Notifications
Notifications
Email notifications will be sent to both office staff and providers whenever an authorization period is coming to an end.
Payer validation
Payer validation
When creating new authorizations, only procedure codes that are covered by the client’s insurance can be selected, ensuring that only procedures or valid combinations of procedures and modifiers allowed by the payer are configured.
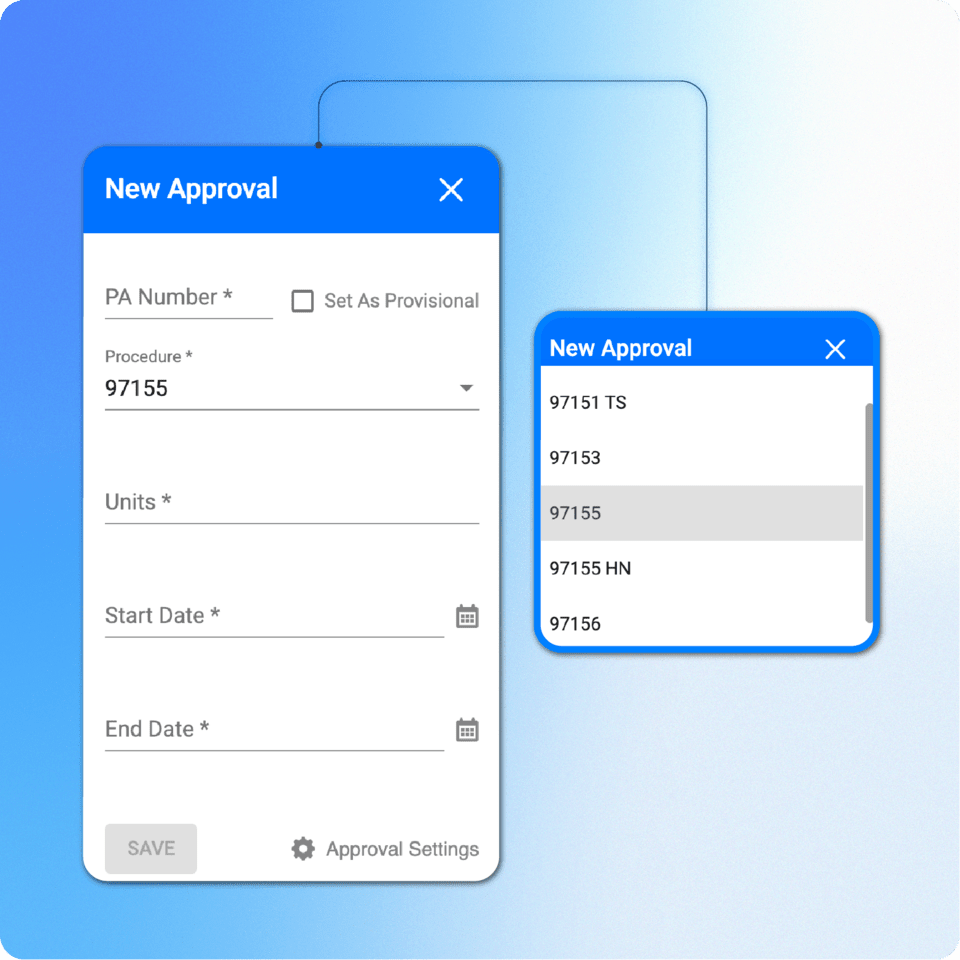
Authorization setup
Authorization setup
In ABA Matrix, users can add prior authorizations (PA) to the client’s profile, including units and approval periods.
Authorization monitoring
Authorization monitoring
Users can monitor remaining authorized units in real time, with seamless integration to the calendar. As sessions are scheduled or updated, the system automatically adjusts the available units, ensuring an always-accurate view of each client’s authorization status.
Overutilization prevention
Overutilization prevention
Users can prevent scheduling or billing when authorized units or periods are exceeded, ensuring that services are always within the coverage limits set by insurance.
Utilization reports and dashboard alerts
Utilization reports and dashboard alerts
Users can access clear reports showing lost hours per week and remaining authorized units, and take a quick glance at the dashboard authorization alerts to keep ahead of any authorization running out of units or expiring.
Notifications
Notifications
Email notifications will be sent to both office staff and providers whenever an authorization period is coming to an end.
Payer validation
Payer validation
When creating new authorizations, only procedure codes that are covered by the client’s insurance can be selected, ensuring that only procedures or valid combinations of procedures and modifiers allowed by the payer are configured.
Stay in control of every authorization
Connect with us and see how ABA Matrix can simplify your workflow